Keeping 2 million nursing facility staff and 1.2 million residents current on their COVID-19 vaccines is one tool for reducing deaths from COVID-19 as the virus continues to evolve. KFF analysis found that despite over one-fifth of all U.S. COVID-19 deaths occurring in long-term care facilities, as of January 14, 2024, only 38% of residents and 15% of staff were “up-to-date” with their COVID-19 vaccines, which the CDC defines as having received the updated Fall 2023 vaccine. Those rates are lower than uptake was for the 2022 vaccine. This data note also finds lower uptake rates for for-profit facilities and state uptake rates that vary from 20% to 63%. Data for this analysis include 14,318 nursing facilities (96% of all nursing facilities, home to 1.2 million residents) that had reported COVID-19 vaccination data as of January 21, 2024.
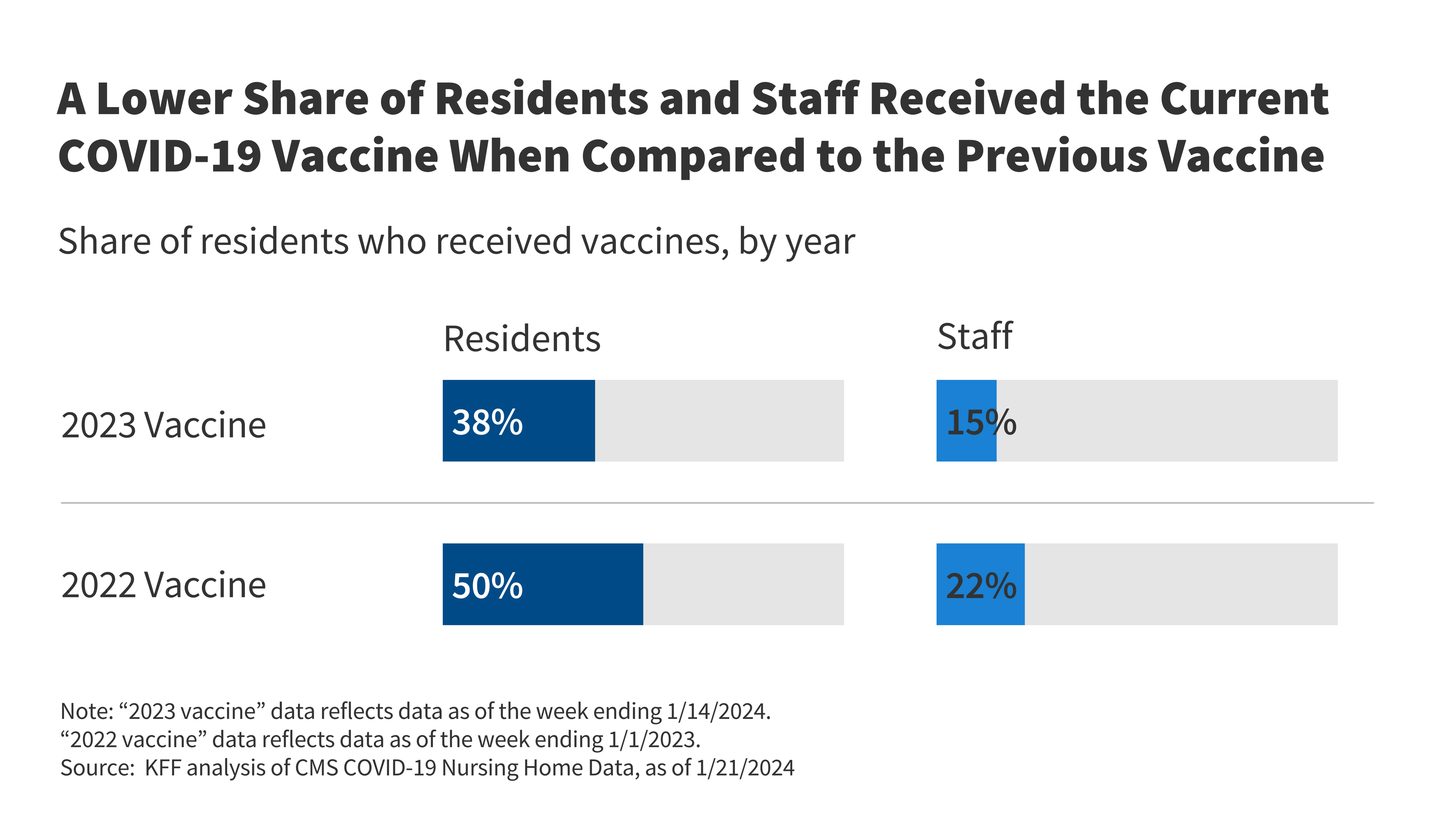
Uptake of the most recent COVID-19 vaccine is lower among nursing facility residents and staff than uptake was for the fall 2022 vaccine: Only 38% of residents and 15% of staff have received the new vaccine (Figure 1). In comparison, at the same point in time last year, 50% of residents and 22% of staff had received the updated vaccine. Those rates represent the share that received the newly available COVID-19 vaccines, 18 weeks after each shot was made available to the public. These rates are much lower than the 87% of residents and 88% of staff who received their primary vaccination series when measured in September 2022. On January 1, 2024, the CDC changed the way it collects data to calculate the percent of staff who are up to date with their COVID-19 vaccination. CMS reports that it may take facilities some time to adapt to the new methodology.
Uptake of the current COVID-19 vaccine is higher in non-profit facilities than in for-profit or government facilities (Figure 2). The percentage of nursing facility residents who received the updated vaccine is 46% in non-profit facilities compared with 35% in for-profit facilities and 43% in government facilities. Uptake of the fall 2022 vaccine was also highest in non-profit facilities and lowest in for-profit facilities. Rates of vaccine uptake for nursing facility staff were low in all types of facilities with minimal variation across facility types (data not shown).
The percentage of nursing facility residents who received the latest COVID-19 vaccine ranges from 20% in Arizona to 63% in Vermont and North Dakota (Figure 3). In eleven states, half or more of nursing facility residents received the newest vaccine while in two states, 25% or fewer have received the most recent vaccine. Uptake among staff of the most recent vaccine ranges from 5% in Arkansas to 51% in Washington D.C. In 42 states, fewer than 20% of staff have received the most recent vaccine. There are a number of factors that may contribute to the variation in nursing facility vaccine uptake across states including ownership patterns and partisanship, with higher rates in states that have more non-profit facilities and states that voted for President Biden in 2020. Other factors include whether facilities have established programs to keep residents current on their vaccines and the success of those various programs. Additionally, some state variation in staff rates may be attributed to variation in how facilities are adapting to new CMS reporting methodology for staff vaccinations.
Federal vaccine clinics contributed to high initial vaccination rates among nursing facility residents, but without ongoing federal initiatives, uptake of vaccines among nursing facility residents may remain low and vary across facilities. Earlier KFF analysis found that nearly 90% of residents completed the initial COVID-19 vaccination series. High take-up of the primary vaccine series stems from high death rates among nursing facility residents, which contributed to a fear of contracting COVID-19, and a concerted policy effort to vaccinate nursing facility residents, including through federally supported on-site vaccination clinics. According to AARP, federal supports have ended and long-term care facilities now coordinate their own COVID-19 vaccination programs, contributing to greater variation across facilities and lower overall rates.
Recent KFF polling shows that over half of previously vaccinated adults are not worried about getting COVID-19, suggesting that uptake of vaccines among nursing facility staff may remain low in the absence of federal mandates. Among nursing facility staff, initial take-up of COVID-19 vaccines was low until a health care worker vaccination mandate required providers that participate in Medicare and/or Medicaid to be vaccinated. This mandate was not updated to include follow-up vaccines, which may contribute to lower uptake of new vaccines among staff, particularly as concern about contracting COVID-19 drops among the U.S, population more broadly.
As winter viruses circulate, COVID-19 vaccines may help decrease sickness and preventable deaths among nursing facility residents and staff. Though people living and working in nursing facilities have likely built some immunity against COVID-19 through prior vaccinations and natural immunity, periodic vaccines have been shown to decrease mortality and increase antibody concentrations among nursing facility residents. For older adults—who constitute most people who use nursing facilities—the risks of COVID-19 may be seven times higher than that of the flu. The CDC finds that 72% of residents had received the flu vaccine as of December 10, 2023, among the small number of nursing facilities that had reported such data, a rate that is nearly twice that of the most recent COVID-19 vaccine. Beyond the flu and COVID-19, RSV is another high-risk respiratory virus. Although there is a new vaccine for RSV, uptake of the new vaccine among nursing facility residents has been hampered by shortages of RSV vaccines and the prioritization of the vaccine for infants and high-risk children. Increasing access to all vaccinations for this population may be a key strategy to preventing respiratory illnesses.