Demographics and characteristics of survey respondents
In total, 1714 individuals were contacted by email with a 39% response rate and for these responses there was a 95% completion rate in taking the survey. Subsequent additional targeted recruitment and outreach via social media especially Twitter (now X) and Facebook resulted in an additional 1,166 respondents starting the survey. In total, 1774 participants answered at least one question and 1310 finished the survey. Of the survey respondents, 688 asked to be included as having contributed to the survey, and they are listed (Supplementary Data File 1).
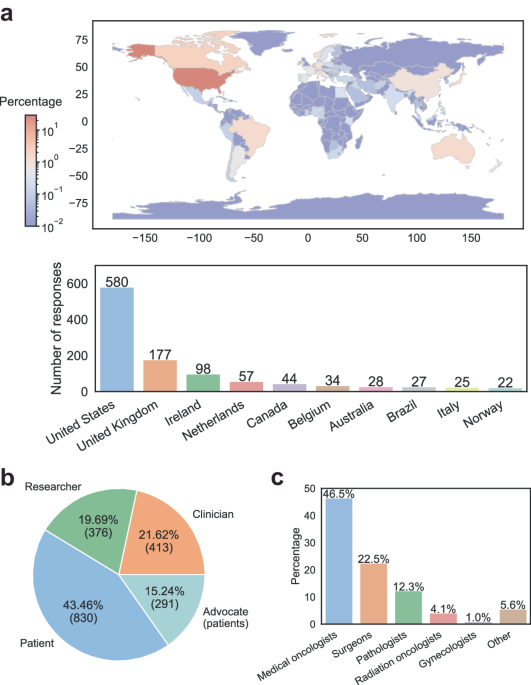
Respondents resided in 66 countries (Supplementary Data File 2) covering all continents except Antarctica (Fig. 1A). The top three countries based on number of respondents were the US (47.65%), UK (9.66%) and Ireland (6.55%).
A A world map showing the percentage by country of respondents to the survey, and the top ten countries with numbers of respondents. World map was generated using B Overall number of physicians, lab- based researchers, and breast cancer patients, with advocates being indicated. C Physicians are separated by clinical specialty.
Respondents self-identified as breast cancer physicians/researchers (N = 413), as basic (laboratory-based) researchers (N = 376), and breast cancer patients (N = 1121) of whom 288 (26.1%) indicated membership in advocacy groups (Fig. 1B). Some respondents belonged to more than one category – 28 clinicians and 17 laboratory-based researchers were also breast cancer patients. There was also overlap between the breast cancer clinicians/researchers and the laboratory-based researcher, with 195 (47.2%) identifying as clinicians with a research lab.
The majority of the breast cancer physicians were medical oncologists (46.5%) and surgeons (22.5%) followed by representation from pathology (12.3%), radiation oncology (4.1%), gynecology (1.0%) and others (5.6%), which included palliative care, patient navigators, clinical oncology, geneticist, family medicine, nuclear medicine and more (Fig. 1C). Most of the clinicians practice in academia (60.6%), followed by private practice (17.4%), and governmental institutions (16.9%). There was an equal distribution of experience: 1–10 years (24.0%), 11–20 years (32.6%), 21–30 years 22.7%), and 31 years and more (19.6%). The majority of physicians treated 11-50 (42.8%) and 51–100 (26.8%) patients per month.
The majority of self-identified laboratory-based researchers work in academic institutions (80.7%), and others in private (9.4%) and governmental (6.7%) institutions. There was a roughly equal distribution of researchers working (50.9%) vs. not working on lobular (49.1%) breast cancer, and 80% of those working on ILC have previously received funding for their work on ILC from a wide range of funders (Supplementary Data File 3). The majority of researchers have been working for 1–10 years (35.7%), followed by 11–20 years (29.7%), 21–30 years (23.7%), 31 years (7.8%) and more (19.6%), and less than 1 year (3.6%).
There were 1121 respondents that indicated that they have or have had breast cancer or in situ carcinoma, called “patients” hence forth. At the time of response to the survey, 62.5% had breast cancer but were currently without evidence of disease, 25.4% were in active treatment for breast cancer, and 19.1% had indicated that their disease had recurred with 8.1% being local and 11.1% being distant recurrences. Lobular breast cancer was the most common histology (63.1%), followed by LCIS (13.6%), DCIS (6.8%), NST (6.3%), mixed ductal/lobular (5.3%) and others/unknown (4.9%). The average age for diagnosis was 52.3 years.
Of the 1121 patients who responded, 288 (26.1%) indicated membership in advocacy groups. Of the total number of respondents to the survey, 403 (23.1% of all respondents) belonged to one or more of 170 different advocacy groups, support groups, and other foundations (Supplementary Data File 4).
Current understanding of lobular breast cancer by clinicians, and communication with patients
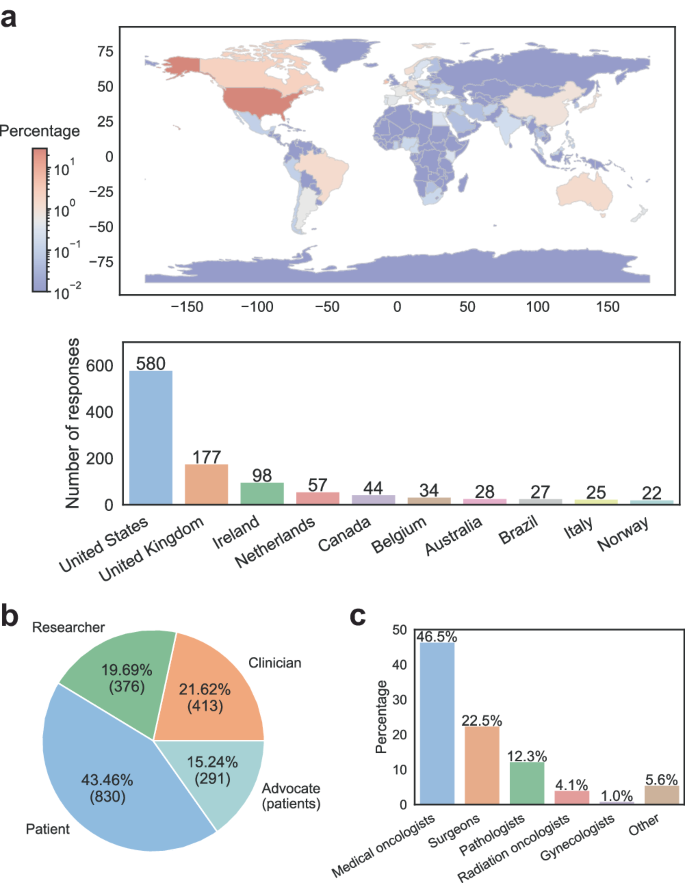
The majority of physicians were confident in describing the differences between ILC and NST (Fig. 2A), and there was no significant difference between medical oncologists, surgeons and other specialties. Only 4% were not all confident, or slightly confident (12%) about the differences. Physicians indicated that knowledge of histology was seen as very/extremely important (73%) (Fig. 2B), and this again was not different between the different specialties The majority of physicians stated that knowledge of histology affected their treatment decisions a lot (51%) or a moderate amount (32%), with surgeons (60%) and others (59%) using histology information significantly more than medical oncologists (40%). Very few physicians (4.5%) felt that knowing histology was not at all or only slightly important. The majority of physicians (57%) indicated that there either was no data, that they did not know, or that they were unsure if there were clinical trials and outcome data supporting unique treatments for ILC. Refining treatment guidelines specifically for lobular breast cancer was seen as valuable for treating patients with ILC in the future by 76% of physicians, for a number of reasons outlined in Supplementary Text File 2.
A Responses by clinicians about confidence in describing differences between ILC and NST. B Importance of knowledge of histology for physicians. C Patients’ responses on communication with physicians. ”Other” refers to “I was not offered personalized therapy because my physician explained that the treatment is no different for ductal than for lobular”.
We asked how patients perceived the knowledge of and specifically, the communication about ILC-specific features by physicians. Many patients (52%) thought that their health care providers did not explain unique features of ILC (Fig. 2C). “Personalized therapy based on histological diagnosis” was discussed with 21% of patients, while it was not discussed with 42%. For 28% of patients, the physicians explained that there was no difference in treatment for NST and ILC. Discussions about potential personalized therapies were held mostly with medical oncologists (89%), followed by surgeons (72%). There were an equal number of radiation oncologists who “definitely did not/probably not” (50%) and who “definitely did/probably did” (50%) discuss ILC-personalized therapy. Most physicians (71%) did not mention that ILC can metastasize to unique places and did not discuss what symptoms, including unusual symptoms, of recurrence the patients should report in the future (78%). For all these communication-related questions, there were differences between countries, with health care providers in the US more frequently being perceived as explaining ILC specific features compared to other countries (Supplementary Data File 5).
Finally, we asked which other ILC-related topics the patients wished they have had a chance to discuss with their physicians. The most common was a discussion of the unique clinical features of ILC, followed by information on recurrence and metastasis, cancer detection and screening, and influence of breast density (Supplementary Data File 6, and Supplementary Fig. 1). All answers were clustered into one of the topics based on semantic similarity, which can be interactively visualized under ‘Topic’ coloring scheme via https://atlas.nomic.ai/data/chelseax488/ilc-survey—discussion-with-doctors/map.
Current basic/translational research and future priorities identified by survey respondents
For those who self-identified as basic or translational researchers, 48% were very/extremely and 29% were moderately confident in describing differences between ILC and NST. The majority (59.8%) performed none or only a little ILC research with only 20% performing a lot or a great deal of ILC research. Reflecting this, only 23% received funding to work on ILC, and those who focused on ILC were significantly more funded for their ILC work (54%) compared to those who don’t focus on ILC (9%).
There is the need for additional ILC models, as only 11% of respondents found that there were sufficient in vitro and in vivo models for ILC research. 32% of respondents use ILC cell line models in their research, the most common being MDA-MB-134 and SUM44. Majority did not use ILC models due to “lack of facility, resources, or expertise”. 52% of respondents felt that ILC was poorly represented in public genomic datasets, while 69% felt that they were able to obtain lobular breast cancer tissue and/or blood samples from patients with ILC for research.
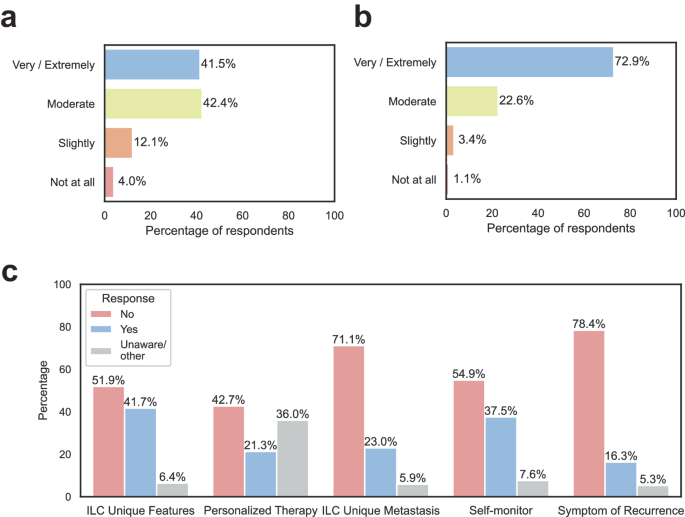
We asked the three major stakeholders for their opinions on research priorities in ILC (Fig. 3, and Supplementary Data File 7). We posed questions about 6 major areas with each area having subcategories. The main areas were: (1) Epidemiology and Risk Reduction; (2) Diagnosis (Imaging and Pathologic Analysis), (3) Therapy, treatment resistance and disease progression; (4) Local therapy of the primary tumor; (5) Imaging; and, (6) Lobular tumorigenesis (the formation of tumors), and other basic/translational research questions. There was general agreement in prioritization of research priorities by the physicians and laboratory-based researchers. Both chose “Therapy, treatment resistance and disease progression” as their top research area followed by “Diagnosis (Imaging and Pathology)”. For 5 out of the 6 areas there was agreement on the specific subcategories of interest with the two highest being “Determining mechanisms of endocrine resistance in ILC” and “Understanding value of genomic predictors for ILC prognosis and prediction of therapeutic response”. The largest discordance was in the area of “Basic/translational research” with physicians choosing “Focusing on development of a centralized ILC data and tissue registry” whereas laboratory-based researchers chose “Characterizing differences in the tumor microenvironment between ILC and NST”. The top priority areas for patients were “Imaging” and “Diagnosis (Imaging and Pathology)”. Within “Imaging”, all groups identified “Identifying new and specific imaging tools for ILC” as the key research area, whereas in “Diagnosis (Imaging and Pathologic Analysis)”, patients chose “Identifying strategies to improve ILC screening/early detection” and physicians and researchers choose “Role of genomic predictors for ILC prognosis and prediction of therapeutic response”.
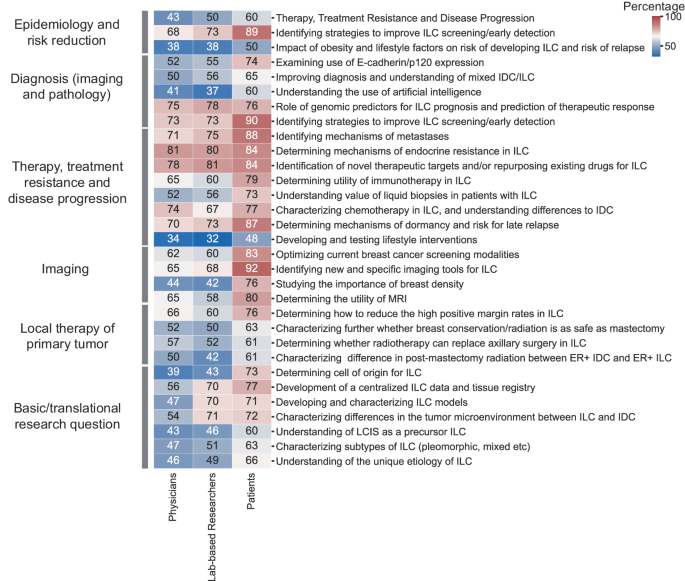
Heatmap showing percentage of individuals rating each research question as of highest importance (‘most critical and impactful’, against moderate/low importance) among 6 domains of topics in physicians, lab-based researchers, and patients, respectively. Color and number represents the percentage from 0-100 in each block.
And finally, there was a free text field question asking which other research questions have high priority that might not have been listed. The most frequently mentioned topics (Supplementary Data File 8) among a wide range of answers were: (1) Genetic screening, Germline mutations, Familial risks, (2) Awareness education, (3) New Aromatase Inhibitors (AI) and Selective Estrogen Receptor Degraders (SERDs) and duration of treatment, (4) Genomic predictors/markers, and, (5) Chemotherapy-related questions.
Clinical trials focused on ILC
Finally, we asked physicians specifically about their opinions on clinical trials in ILC. Half of the physicians reported that “Most of the time/always” approximately half of the clinical trials and studies they were involved in collected data on tumor histology, with twice as many surgeons (35%) than medical oncologists (16%) “always” collecting histology information. Further, 66% of physicians stated that clinical trials they are involved in do not or only sometimes consider histology in their inclusion/exclusion criteria. Most physicians (86%) have not powered clinical trials they were involved in to specifically allow a subset analysis for ILC, and this was not significantly different between surgeons, medical oncologists and other physicians. However, 50% would “probably” and 36% would “definitely” consider powering clinical trials to do subset analysis of lobular breast cancer in the future, for a wide range of reasons (Supplementary Text File 3). Importantly, most physicians (87%) would consider participating in consortia conducting clinical trials in ILC.